Antibiotic stewardship refers to efforts in doctors offices hospitals long-term care facilities and other health care settings to ensure that antibiotics are used only when necessary and appropriate. All healthcare facilities should have antimicrobial stewardship programs in place.
 Core Elements Of Antibiotic Stewardship Global Alliance For Infections In Surgery
Core Elements Of Antibiotic Stewardship Global Alliance For Infections In Surgery
It is important to know that antibiotics only treat bacterial infections not viral infections.

What is antibiotic stewardship. The term antimicrobial resistance is defined as the loss of effectiveness of any anti-infective. Antimicrobial stewardship is a dedicated coordinated program designed to improve antibiotic use while optimizing treatment of infections and reducing adverse events associated with antibiotic use. Scopus 248 Google Scholar.
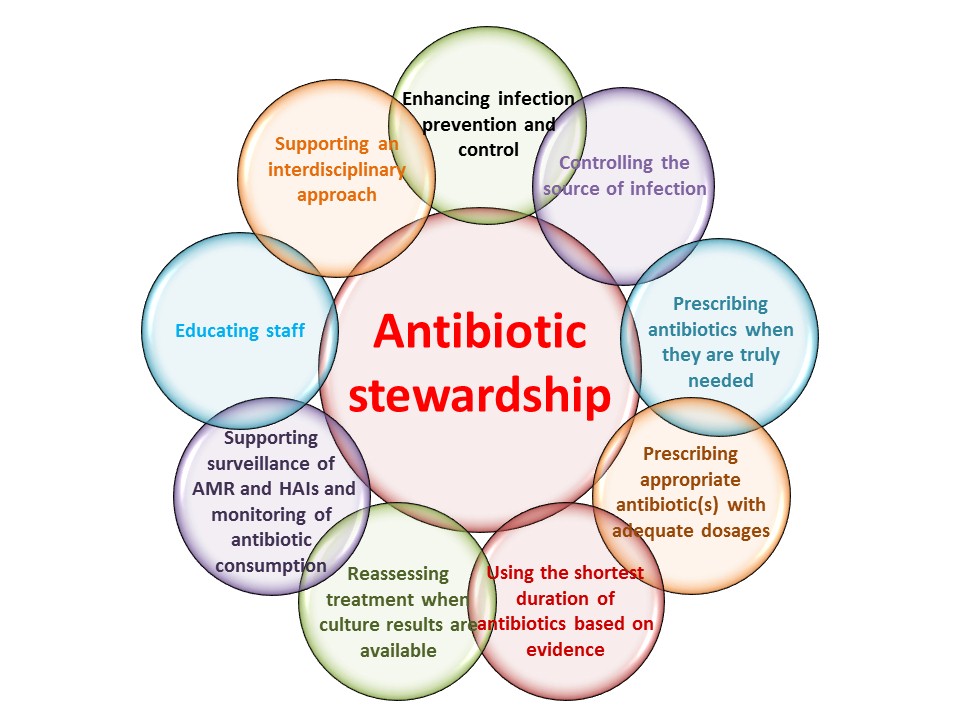
Antimicrobial stewardship is a key component of a multifaceted approach to preventing the emergence of antimicrobial resistance. Antibiotic stewardship refers to a set of commitments and actions designed to optimize the treatment of infections while reducing the adverse events associated with antibiotic use. The term antimicrobial stewardship is defined as an organisational or healthcare-system-wide approach to promoting and monitoring judicious use of antimicrobials to preserve their future effectiveness.
Antimicrobial stewardship is the conservation of antibiotics so they continue to work effectively. Quality standard - Antimicrobial stewardship. Addressing AMR through improving stewardship is a national medicines optimisation priority led by NHS England and supported by PHE.
Antimicrobial stewardship refers to the responsible use of antimicrobials by healthcare professionals and more specifically to selection of the most appropriate antibiotic duration dose and route of administration for a given patient with a demonstrated or suspected infection. Antimicrobial stewardship is a method of overseeing antimicrobial use in healthcare facilities to ensure that every patient requiring antimicrobial therapy receives optimal therapy. Antibiotic stewardship is the effort to measure and improve how antibiotics are prescribed by clinicians and used by patients.
In 2019 CDC updated the hospital Core Elements to reflect both lessons learned from five years of experience as well as new evidence from the field of antibiotic stewardship. Improving the use of antibiotics in healthcare to protect patients and reduce the threat of antibiotic resistance is a national priority. That means prescribing the right drug at the right dose at.
Antimicrobial stewardship is a coordinated program that promotes the appropriate use of antimicrobials including antibiotics improves patient outcomes reduces microbial resistance and decreases the spread of infections caused by multidrug-resistant organisms. Antimicrobial stewardship can help improve patient safety reduce treatment failures ensure correct prescribing of antibiotics and reduce. Stewardship is achieved by promoting the selection of the optimal antibiotic regimen dose duration and route of administration.
Antimicrobial stewardship AMS refers to an organisational or healthcare system-wide approach to promoting and monitoring judicious use of antimicrobials to preserve their future effectiveness. Improving antibiotic prescribing and use is critical to effectively treat infections protect patients from harms caused by unnecessary antibiotic use and combat antibiotic resistance. It aims to change prescribing practice to help slow the emergence of antimicrobial resistance and ensure that antimicrobials remain an effective treatment for infection.
Instead antibiotic stewardship is the call to use antibiotics for the conditions where they are specifically indicated and to use the right choice of antibiotic the right dose route and the right duration. Antimicrobial stewardship refers to interventions designed to promote the optimal use of antibiotic agents including drug choice dosing route and duration of administration. Antibiotic stewardship programs can help clinicians improve clinical outcomes and minimize harms by improving antibiotic prescribing.
This guideline covers the effective use of antimicrobials including antibiotics in children young people and adults. Prescribers should carefully consider if the patients condition warrants an antibiotic. The term antimicrobial stewardship refers to a series of coordinated interventions aimed to promote the appropriate use of antimicrobials and directs the optimal choice of drug dose and duration of therapy and the route of administration.
As a means to tackle resistance. Antimicrobial stewardship is a collective set of strategies to improve the appropriateness and minimise the adverse effects of antibiotic use including resistance toxicity and costs. What is antimicrobial stewardship.
Antibiotic stewardship sometimes referred to as antimicrobial stewardship refers to the efforts made in doctors offices hospitals long-term care facilities and other healthcare facilities to embrace a mentality of only prescribing antibiotics when necessary. This can be accomplished by using antibiotics properly.


